
1) Shimon Rochkind
2) Kimberly Byrnes, Juanita
Anders, et al.
3) Albert Bohbot
4) Margaret Naeser
5) Relevant
Stroke & Head Injury Research
Lasers amplify light by producing coherent light
beams. As a noninvasive, painless mechanism for stimulating regenerative
processes that does not heat tissue, low-energy lasers are finding
numerous therapeutic applications. Scientists speculate that laser
energy alters many physiological processes, including cellular
respiration and gene expression.
Considerable intriguing research is emerging
documenting the potential of laser therapy to treat both peripheral
nerve and spinal cord injuries. For example, in the case of cultured
neuronal cells, laser irradiation induces substantial sprouting and
outgrowth of neurites (i.e., budding axons and dendrites), apparently
via the increased production of several regeneration-stimulating nerve
growth factors.
Overall, animal
studies indicate that laser therapy has a quick neuroprotective effect,
preserves injured nerve functional activity, decreases injury-site scar
tissue, lessens degeneration in corresponding motor neurons of the
spinal cord, and increases axonal growth and myelinization. In cell
cultures, laser therapy accelerates neuronal cell migration, cell
growth, and fiber sprouting.
1) Dr. Shimon Rochkind
(Israel), a pioneering scientist in this area, treated 31 patients
with severe spinal-cord cauda equine injuries (average three years post
injury) with laser therapy six hours daily for 21 consecutive days. Of
these patients, nearly half showed some functional motor improvement.
Rochkind also examined the effects of embryonic
spinal-cord-cell transplantation and laser therapy on recovery after SCI
in rats. Results indicated that the best recovery of limb function and
gait performance, electrophysiological conduction, and histological
parameters (indicating implanted tissue growth) occurred after cell
implantation and laser radiation.
This work is increasingly relevant because several
patients, who have had various
function-restoring cells transplanted into their injured cords, have augmented transplantation
with laserpuncture therapy discussed below.
Other studies on injuries to peripheral nerves
(i.e., nerves outside of the brain and spinal cord) further demonstrate
laser-therapy’s potential neuroregenerative power. For example, Rochkind
examined the effects of irradiation on axonal regeneration across a
transected peripheral nerve bridged with a biodegradable polymer.
Such polymers may ultimately play an important role in paving the
pathway for regeneration in SCI. Briefly, rats were irradiated at the
reconstructed peripheral injury location, as well as the spinal-cord
areas corresponding to the affected peripheral nerves. Compared to
controls, laser-treated rats had more myelinated (i.e. insulated) axons
going across the polymer bridge, signal conduction going through the
axons, and functional recovery.
In another study in humans, Rochkind evaluated the
effectiveness of laser irradiation in patients with incomplete
peripheral nerve injuries or injuries to the
brachial plexus nerves (a nerve
network that conducts signals from the spine to the arms). Specifically,
18 subjects, who had sustained their injuries at least six months
earlier, were randomly assigned to receive either transcutaneous laser
irradiation or treatment from an identical looking placebo device.
Subjects were treated for 21 consecutive days - three hours daily at the
injury area of the peripheral nerve and two hours daily at the
corresponding spinal-cord segments. The subjects were periodically
evaluated for six months. Compared to controls, the laser-irradiated
subjects improved in motor but not sensory function.

2)
Drs. Kimberly Byrnes, Juanita Anders
(photo) and
colleagues (USA) have generated evidence suggesting that laser therapy is
beneficial after SCI. Specifically, their studies demonstrated that
laser irradiation alters gene expression in rats after acute SCI and
exerts an anti-inflammatory effect on the injured cord. As such, it
could reduce secondary injury and, in turn, some of the barriers
inhibiting axonal regeneration. 
Especially relevant to the promising olfactory-tissue transplantation
procedures discussed elsewhere, the investigators have shown that laser
irradiation alters gene expression of regeneratively-endowed olfactory
ensheathing cells (OECs). This alteration enhances the expression of key
growth factors and extracellular matrix proteins that support neuronal
regeneration. The findings support the use of laser therapy in
combination with OEC transplantation.
Recently, the investigative team compared the
effects of laser therapy in rats with injuries created by either 1)
cutting a portion of the cord (i.e., hemisection) or 2) an impact-caused
contusion (the most common sort of injury). Immediately after injury,
rats were irradiated through the skin at the injury site for 14
consecutive days. Compared to controls, laser therapy augmented axonal
survival and re-growth, and functional recovery for both types of
injury.

3) Albert Bohbot
(La Chapelle, Montlinard, France) has developed laserpuncture therapy
which combines elements of acupuncture and laser therapy, both of which
have shown potential for restoring some function after SCI. Although the
use of lasers to stimulate acupuncture points is not new, Bohbot has
developed and refined this technology and directed it towards paralysis.

With the support of a French Government
technology-transfer grant and assistance of scientists at one of France’s
leading engineering universities, Bohbot developed a sophisticated
electronic instrument that substituted an infrared laser light beam for
acupuncture needles. This device specifically emits infrared energy - the
part of the electromagnetic spectrum just beyond the limit of visible red
light.
Central to laserpuncture therapy is a network of more
than 300 acupuncture points Bobhot elucidated based on many years of
study, including the examination of ancient Chinese texts. This network
relates acupunctural energy meridians to dermatome levels. Bohbot believes
that the stimulation of energy through this network restores some
function.
Because laserpuncture therapy seems to have restored
significant function in many with supposedly complete clinical injuries,
Bohbot speculates it is possible to restore some function without intact
neurons bridging the spinal injury site. Substituting prevailing
biomedical dogma with innovative explanations involving quantum physics
and energy medicine, Bohbot believes that there are backup mechanisms to
the spinal cord for carrying messages from the brain to the body. He
suggests that a signal may be mediated through an electromagnetic energy
impulse instead of standard, biochemical conduction through intact neurons
using neurotransmitters. In fact, Traditional Chinese Medicine suggests
that energy interactions are possible above and below the injury site.
Regeneration may also be due to the turning on of
residual, but dormant, neurons that have survived the injury. Scientists
now believe that such dormant neurons characterize many injuries
clinically classified as “complete” and only a few of these neurons to be
turned on to regain some function. Perhaps laserpuncture is a therapeutic
switch that turns them on.
Bohbot has treated many people with SCI, most of whom
were at least a year post-injury. Many claim to have regained significant
function.
The sessions are augmented with more traditional
physical rehabilitation designed to enhance restored function. Bohbot and
colleague Dr. Cécile Jame-Collet studied the effect of this laserpuncture
program in 22 individuals with SCI (both paraplegia and quadriplegia) and
found that over time, the program increased both thigh and calf
circumference.
Bohbot’s patients include those who have been
recipients of transplanted, regeneratively endowed cells or tissue,
including olfactory ensheathing cells (OECs), patient-derived olfactory
tissue, and bone-marrow-derived stem cells.
In a recent article, Bohbot evaluated the functional improvements by
electromyography (electrical recording of muscle activity) of three
individuals who underwent Dr. Huang’s OEC transplantation procedures. As
discussed elsewhere, OECs theoretically promote axonal
regeneration by producing insulating myelin sheaths around both growing
and damaged axons, secreting growth factors, and generating structural
and matrix macromolecules that lay the tracks for axonal elongation.
Bohbot’s results suggested that the laserpuncture/cell-transplantation-combination
therapy restored some voluntary muscle activity.

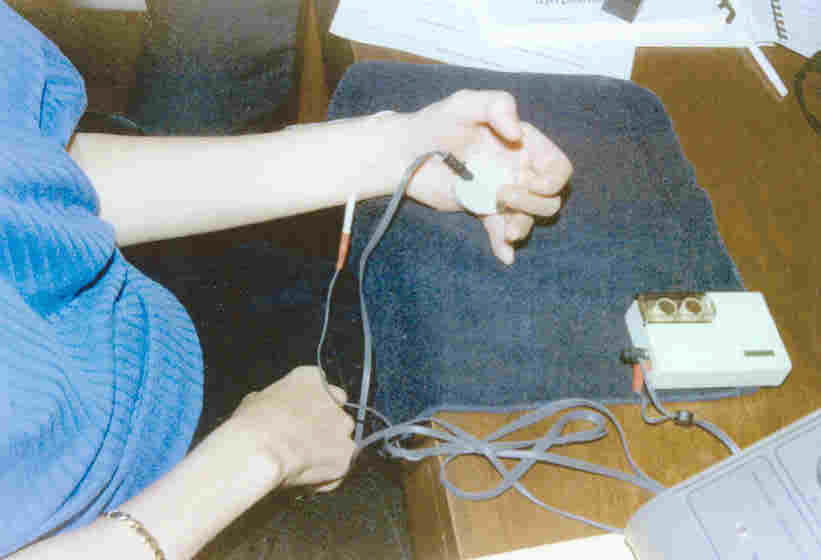
4)
Dr.
Margaret Naeser and colleagues (Boston, Massachusetts, USA) have
developed an effective therapy for SCI-associated carpel tunnel syndrome
(CTS) and spasticity-related hand-flexion problems. Naeser’s therapy
specifically stimulates hand acupuncture points with a low-energy laser
beam and a mild electrical current. Specifically, the therapy uses 1) a
laser pointer powered by two AAA batteries and 2) microamps transcutaneous
electrical nerve stimulation (TENS) using a MicroStim 100 TENS device.
Naeser’s approach is supported by rigorously designed
clinical studies. These studies indicate that approximately 90% of
individuals with mild-moderate CTS treated with her program three times a
week for 4-5 weeks by a licensed acupuncturist will have significant,
enduring relief from CTS pain (Arch Phys Med Rehabil 83, 2001).

5)
Stroke & Head Injury:
With relevance to SCI, laser therapy’s neuroregenerative influences are
further documented by stroke and head-injury research. For example, evidence
indicates that laser therapy improves outcomes to some degree after
ischemic stroke (neurological damage caused by interruption of brain’s
blood flow). Specifically, in an international, multicenter clinical
trial, 120 patients were randomized to receive transcranial laser
therapy (i.e., through the skull) or treatment from a sham device
emitting no laser energy within 24 hours of stroke onset. After 90 days,
70% of the laser-treated subjects had improvements compared to only 51%
of the controls.
In a more recent, larger study, 660 patients with
acute ischemic stroke were randomized to receive either transcranial
laser therapy or sham treatment. In the laser-treated group, 120
achieved a favorable outcome compared to 101 in the control group.
Regarding head injury, Dr. A. Oron and
colleagues (Israel) have shown that transcranial laser therapy reduces
head injury in rats when administered four hours after trauma.
TOP