(With permission of the publisher, adapted from
articles appearing in "PN/Paraplegia News
Magazine" by Lisa Hudgins, Paralyzed Veterans
of America)
The human nervous system is responsible for sending,
receiving, and monitoring all nerve impulses or signals. These electrical
and chemical signals are required to organize everything we do - from
thinking about a problem, to digesting a meal, to throwing a baseball, to
sweating when hot. Anatomically, the nervous system is divided into two
main sections: the central nervous system (CNS) and the
peripheral nervous system (PNS). The CNS, the main processor of I
information, includes the brain and spinal cord. The PNS involves those
parts of the nervous system outside the brain and spinal cord, and it
connects the CNS to the body's organs and extremities. The PNS is
responsible for executing commands issued by the CNS and relaying
information from the body and the outside world back to the brain and
spinal cord.
The nervous system also has two functional divisions:
the somatic and the autonomic nervous systems. These systems are
predominately located within the PNS. The somatic nervous system is
involved in the control of mostly voluntary activities, such as tapping
your foot to music. The autonomic nervous system (ANS) connects the CNS to
the internal organs and glands of the body and is involved in regulating
involuntary functions such as heartbeat. The ANS has two subdivisions: the
sympathetic and the parasympathetic systems. The sympathetic nervous
system mobilizes energy and resources during times of stress and arousal,
while the parasympathetic conserves energy and resources during relaxed
states.
It may sound confusing to have so many different
divisions in the nervous system, each called a "system." The main thing to
remember is that the nervous system has divisions based on where the
nerves are (CNS and PNS) and what they do (somatic and autonomic). The
sympathetic and parasympathetic systems are part of the ANS.
As noted, the CNS is made up of the brain and spinal
cord, which are connected. The spinal cord contains bundles of nerves that
extend from the brain down the back and serve as sort of a communications
cable relaying information to and from the brain and the rest of the body.
It is encased in a series of membranes called the meninges (when they
become infected, the condition is called meningitis). The membrane
attached directly to the spinal cord- the pia mater- contains the cord's
blood supply. Surround-
ing the pia mater is a liquid called cerebrospinal
fluid (CSF), which acts to cushion the spinal cord. The CSF is held in
place by a second membrane – the arachnoid. The last, outer membrane, the
dura mater, is tough and fibrous.
A BONY TUNNEL
Although it is a critical part of the nervous system,
the spinal cord is relatively small (about 18 inches long and the width of
your little finger) and fairly fragile. To prevent it from being easily
damaged, it is housed inside a bony tunnel called the spinal or vertebral
canal. Twenty-nine vertebrae or back bones stack on top of each other to
make up the
spine or vertebral column. Each of these oddly shaped
vertebra has a hole in it. When the bones are stacked on top of each
other, the vertebral foramen [opening, orifice, or short passage] of each
one lines up to form the vertebral or spinal canal through which the
spinal cord runs. When stacked, the spaces form a tunnel that protects the
spinal cord. Because of all the bending and lifting people's backs must
do, each vertebra is cushioned from the next one by a spongy cartilage
disc that acts as a shock absorber. Ligaments connect all the vertebrae to
one another so that the bones of the spine can remain properly aligned and
move in a coordinated fashion.
The spine has four main sections. The first seven
bones, cervical vertebrae, make up the neck. The next 12, the thoracic
vertebrae, extend to about the waist (each of the 12 ribs is attached to a
thoracic vertebra in the back). In the lower back area are five lumbar
vertebrae. Below these is the sacrum, a flat v-shaped bone (made of five
fused vertebrae) that anchors the spine to the pelvis or hip bones. At the
very end of these four main sections is a small tailbone, the coccyx, also
made up of fused vertebrae.
CONTROL SYSTEM
At each vertebral level, spinal nerves project off
the left and right sides of the spinal cord to every part of the body
through openings in the vertebral column (click on thumbnail). At every
level, spinal nerves branch off both sides of the spinal cord to supply
innervation [distribution of nerves] to the entire body. There are 31
pairs of spinal nerves in all. Each pair provides innervetion to the left
and right sides of a segment of the body. Like the vertebrae, the spinal
nerves are named according to level: 8 cervical spinal nerves, 12 thoraci c,
5 lumbar, 5 sacral, and 1 coccygeal. Because the spinal cord itself is
shorter than the spine (ending far above the tailbone), the lumbar,
sacral, and coccygeal spinal nerves develop long extensions to exit the
corresponding level of the vertebral column. These long spinal nerve
extensions are distinctive in appearance and are collectively called the
cauda equina (Latin for "horse's tail"). Because the spinal cord ends far
above the tailbone, long extensions, collectively called the cauda equina,
are required to reach the lower segments of the spine.
c,
5 lumbar, 5 sacral, and 1 coccygeal. Because the spinal cord itself is
shorter than the spine (ending far above the tailbone), the lumbar,
sacral, and coccygeal spinal nerves develop long extensions to exit the
corresponding level of the vertebral column. These long spinal nerve
extensions are distinctive in appearance and are collectively called the
cauda equina (Latin for "horse's tail"). Because the spinal cord ends far
above the tailbone, long extensions, collectively called the cauda equina,
are required to reach the lower segments of the spine.
Each spinal nerve is attached to the cord by
structures called dorsal and ventral roots (Click on thumbnail). On each
side, a dorsal root carrying sensory information to the CNS and a ventral
root carrying motor information from the CNS connect to form a spinal
nerve. Ventral roots leaving the cord contain motor (pertaining to
movement) fibers; whereas, dorsal
 roots
entering the cord contain sensory (pertaining to feeling) fibers. These
spinal roots mark the beginning of the PNS. At every level, one ventral
and one dorsal root on each side of the body come together to form a
spinal nerve. Each spinal nerve then divides repeatedly like the branches
of a tree until the entire body is innervated.
roots
entering the cord contain sensory (pertaining to feeling) fibers. These
spinal roots mark the beginning of the PNS. At every level, one ventral
and one dorsal root on each side of the body come together to form a
spinal nerve. Each spinal nerve then divides repeatedly like the branches
of a tree until the entire body is innervated.
Nerves within the spinal cord that are involved in
controlling movement are called upper motor neurons (UMNs), whereas nerves
that leave the spinal cord to connect to muscles are called lower motor
neurons (LMNs). Each "nerve" in the body is not a single nerve but rather
a collection of many individual sensory and motor nerve cells or neurons.
There are many different types of neurons with many different shapes and
structures. The typical neuron has three main regions: a cell body,
dendrites, and an axon (Click on thumbnail). The cell body is the
metabolic or manufacturing center of the neuron. It is responsible for
making the nutrients and structures necessary for the neuron to live and
function. Dendrites are fine tubular
extensions that radiate fr om
the cell body like antennae and are the major receptors of information
from other cells. The axon (also called the nerve fiber) is a long stem
that extends away from the cell body. It conducts neuronal signals from
the nerve cell to distant targets in the body, such as muscles, organs, or
other nerves. Neuronal signals are transmitted from one cell to another at
junctions called synapses.
om
the cell body like antennae and are the major receptors of information
from other cells. The axon (also called the nerve fiber) is a long stem
that extends away from the cell body. It conducts neuronal signals from
the nerve cell to distant targets in the body, such as muscles, organs, or
other nerves. Neuronal signals are transmitted from one cell to another at
junctions called synapses.
Most larger neurons make use of a special insulation
called myelin to maximize the conduction of the nerve signal down their
long axons. Myelin is insulation that surrounds the axon of many nerves.
This myelin sheath helps the nerves conduct impulses and is required for
proper function. The sheath wraps around the axon to prevent signal
leakage and increases the speed and efficiency with which the signal is
transmitted. Because myelin is w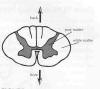 hite,
the spinal cord appears two-toned in color when cut in half
(cross-section). Gray matter, which looks somewhat like a butterfly, is
found in the center of the cord and contains clusters of cell bodies.
White matter surrounds the gray matter and contains bundles of myelinated
axons (Click on thumbnail). Specialized cells called oligodendrocytes and
Schwann cells form myelin. Both of these are types of glia.
hite,
the spinal cord appears two-toned in color when cut in half
(cross-section). Gray matter, which looks somewhat like a butterfly, is
found in the center of the cord and contains clusters of cell bodies.
White matter surrounds the gray matter and contains bundles of myelinated
axons (Click on thumbnail). Specialized cells called oligodendrocytes and
Schwann cells form myelin. Both of these are types of glia.
Another class of cells called glia (Greek for
"glue"), or glial cells, are nerve support cells found between neurons and
the blood vessels supplying the nervous system; they outnumber nerve cells
by at least ten to one. Although they do not generate electrical signals
like neurons, glia provide important mechanical support for nerve cells
and have other vital functions as well.
In addition to providing myelin for neurons, glia may
also supply nutrients for the nerve cells, guide and direct axon
outgrowth, maintain chemical balance in the environment surrounding the
neurons, and clear out debris after neuronal death or injury. The main
glial cell in the PNS is the Schwann cell, and the main glia in the CNS
are the oligodendrocyte and the astrocyte. Damage or disease to either the
nerve cells themselves or to the glia can result in a loss of function in
humans.
HOW PARALYSIS BEGINS
SCI can result from damage to the vertebral column or
to the spinal cord itself. Most SCIs occur when trauma or injury to the
vertebral column causes a fracture of bones or a tearing of ligaments. .
Either can result in a displacement of the bones of the spine, which in
turn can lead to SCI. Bone displacement can cause spinal-cord bruising
(contusion), pinching (compression), stretching (distraction), or some
combination of these.
In rare instances, injury to the vertebral column
will result in an actual cutting or penetration of the spinal cord.
Penetrating SCIs more often are due to gunshot or stab wounds that mayor
may not damage surrounding vertebrae. SCI can also be caused by ischemia,
a decrease or loss of blood flow to the cord. This can happen as a result
of injury, disease, or certain surgical procedures, particularly those
involving clamping the aorta. Fortunately, SCI from surgery is very rare.
Because the causes of SCI vary greatly, no two
injuries are exactly alike. However, the basis of the resulting paralysis
is the same: the death of neurons, and the disconnection and demyelination
of axons. Thanks to research, scientists can generally describe the
pathology (deviations from normal anatomy) and pathophysiology (abnormal
biological and chemical processes) responsible for these changes, although
they are still not completely understood.
At the time of injury, neurons, glia, and blood
vessels in the injury zone experience an initial mechanical damage.
Following this "primary" injury, several mechanisms become operative. This
leads to further damage, called "secondary" injury, which is often
responsible for more of the functional deficit people with SCI experience
than is the initial trauma itself.
The progression of secondary injury can vary greatly
depending on the severity of the initial trauma. Typically, after a
moderately severe trauma, secondary injury begins within 30 minutes with
hemorrhage or bleeding in the central gray matter of the spinal cord. Over
the course of several hours, this hemorrhage radiates outward to include
surrounding white matter as well. Within two hours of injury, a
significant reduction of blood flow (ischemia) occurs in the region.
Within six hours, edema (swelling) is visible in the area. The edema,
hemorrhage, and ischemia all result in decreased oxygen supply (hypoxia)
in that region of the spinal cord, which leads to the death (necrosis) of
local tissue.
Also about two hours after injury, inflammatory cells
begin their invasion. These immune-system cells protect us from disease
and infection by killing harmful bacteria in our body and clearing away
waste and debris. By the fourth hour, some of these inflammatory cells
begin killing the damaged nerves in the spinal cord.
All of the events described above ultimately lead to
further nerve damage in the spinal cord. If the initial trauma is severe,
the secondary-injury process may begin immediately, and the entire injury
zone can become filled with dead or necrotic tissue within 48 hours.
However, immune-system cells eventually clean up the area by removing all
the dead tissue. Several weeks after the initial trauma, only a cavity
and/or scar tissue remain at
the injury site. However, even in the most severe.
injuries, surviving neurons cross the injury zone along the perimeter of
the spinal cord. Although these neurons are intact, they are damaged,
demyelinated, and nonfunctioning.
INJURY CLASSIFICATION
Each SCI is different, and each is described by its
type ("complete" or "incomplete") and level. In general, "complete" means
no voluntary movement or sensation exists below the injury level. Some
feeling or voluntary movement remains in an "incomplete" injury. A British
neurologist, Dr. Frankel, developed a more detailed system of
classification of neurological function. The American Spinal Injury
Association (ASIA) subsequently refined this scale, which grades injuries
from "A" (a complete injury) to "E" (recovery). The International Medical
Society of Paraplegia (IMSOP) adopted the refined ASIA
Impairment Scale, which is now the international
standard for classification of neurological function.
ASIA
IMPAIRMENT SCALE
ASIA and IMSOP have also developed standardized
classifications for levels of SCI. According to these standards, the
neurologic level of injury is defined as "the most caudal (lowest) segment
of the spinal cord with normal sensory and motor function on both sides of
the body." The generic way that level of injury is described is by the
classifications "quadriplegia or tetraplegia," referring to injuries of
the cervical regions, and “paraplegia," referring to injuries of the
thoracic, lumbar, or sacral regions.
In general, after SCI the nerves above the level of
injury continue to work normally; those below it are impaired.
Consequently, the parts of the body innervated by the nerves below the
level of injury don't function the way they used to. In fact, some parts
may no longer operate at all.
Because the spinal cord connects with all the body's
nerves, damage to it can alter every system. In addition to affecting a
person's ability to move and feel, SCI can affect skin, breathing,
bladder, bowel, sexual function, and subconsciously controlled phenomena
like blood pressure and sweating.
Earlier, it was explained that spinal-cord nerves
that control movement are called upper motor-neurons (UMNs); nerves that
leave the spinal cord to connect with muscles are lower motor-neurons (LMNs).
More specifically, axons from nerve-cell bodies in the brain run inside
the white matter of the spinal cord to connect with specific nerve-cell
bodies (motor neurons) in the gray matter. The axons from these motor
neurons then leave the cord to make connections with the muscles in the
body. UMNs, which originate in the brain, regulate and control the
movement stimulated by LMNs, the nerves that originate in the spinal cord.
In a UMN injury, control by the brain no longer
exists because messages from the brain are cut off at the point of SCI.
Therefore, LMNs react without limit or inhibition, causing uncontrolled
muscle contractions. This is called spasticity, and an UMN injury is said
to result in "spastic" paralysis. On the other hand, LMN injuries cause a
"flaccid" paralysis because muscles of the limbs get cut off from nerves
that supply them. This lack of innervation causes muscles to become limp
or flaccid. Muscle spasms can either be "alternating" (producing twitching
or shaking) or "sustained" (causing rigidity in the limbs). All spasticity
represents the activity of uncontrolled reflexes of the LMNs and is the
result of the brain's loss of control over the somatic nervous system.
Another example of uncontrolled reflexes is autonomic
dysreflexia (AD) - the lack of the brain's control over the autonomic
nervous system. AD is a serious condition that may occur in individuals
with SCI at T6 or above. Before SCI, a stimulus below the level of injury
would have signaled pain or discomfort from such things as a full bladder,
sun-burn or labor contractions. After SCI, These conditions can cause AD,
which, if not treated promptly, can lead to stroke and is potentially life
threatening.
TOP